by Kathie Lipinski, RN, MSN, CH
Author’s note: This article follows my presentation at the International Center for Reiki Training Annual Retreat at Lake George, New York 2012. At the time of this writing, we on the northeast coast of the United States have just lived through Hurricane Sandy and a nor’easter. This article first appeared in the Winter 2012 issue of Reiki News Magazine.
Many residents along the East Coast, especially here on Long Island where I live, are in the midst of Post-Traumatic Stress Disorder as they struggle to survive and have their basic needs met (from hurricane Sandy). Their story of survival, heroism and community coming together is a work in progress and a tribute to the strength and resilience of the human spirit.
 Post-Traumatic Stress Disorder: The dark night of the soul
Post-Traumatic Stress Disorder: The dark night of the soul
With today’s technology and communication systems, it is easy to become aware of world events as well as individual experiences. What was once experienced locally can now be shared globally. Trauma, often times part of the human condition, whether experienced individually or collectively, can now be experienced vicariously through the Internet and/or television. It is no wonder that awareness of Post-Traumatic Stress Disorder (PTSD) has risen dramatically and information about this condition is much more readily available (See Resources). PTSD is still an individualized experience, with ramifications for the family as well as the community. It is an injury of the soul and the spirit of the person. Reiki can calm and restore the spirit, often times bringing healing to old, buried wounds.
My attempt in writing this article is to provide a general description of PTSD, its causes and symptoms, and most important, how we as Reiki practitioners can help. I have also included guidelines provided me through my experiences working with people with PTSD as well as those of the nurses who work with veterans at the Northport VA Medical Center here on Long Island as part of the 2011 Mind-Body Grant. It is beyond the realm of this article to discuss the entire scope of PTSD, including factors such as statistics, susceptibility, causes, risk factors, diagnosis and treatment. Instead, I have included a list of excellent resources that provide that pivotal information.
Post-Traumatic Stress Disorder defined
The term PTSD was first coined in 1980 when the American Psychiatric Association (APA), the main professional organization of psychiatrists in the United States, added PTSD to their DSM classification (Diagnostic and Statistical Manual of Mental Health Disorders). The DSM is the standard classification of mental disorders used by mental health professionals in the United States. Their intention was to fill a gap in psychiatric theory and practice.
The most current edition of the DSM-IV-TR 2000 lists the criteria for the diagnosis of PTSD as:
309.81 Posttraumatic Stress Disorder
The person has been exposed to a traumatic event in which both of the following were present:
- The person experienced, witnessed or was confronted with an event or events that involved actual or threatened death or serious injury, to a threat to the physical integrity of self or others.
- The person’s response involved intense fear, helplessness, or horror (note in children this may be expressed by disorganized or agitated behavior)
- The disturbance causes clinically significant distress or impairment in social, occupational or other important areas of function.
- The symptoms usually develop shortly after the event but may take years
- Symptoms are present for at least one month.
- It is considered an anxiety disorder.(1)
The classification by the DSM was important because it emphasized that the causative agent of PTSD was outside the individual (i.e. traumatic event) rather than an inherent weakness. The classification was revised in 1987, 1994, and 2000 (next edition due out in 2013), as they came to understand that different people have different perceptions of trauma as well as different responses or vulnerability to developing symptoms after being exposed to extreme stressful events or situations.
One important finding that was not apparent when PTSD was first proposed as a diagnosis in 1980 is that it is relatively common. Recent data from the National Comorbidity Survey indicates PTSD prevalence rates are 5% and 10%, respectively, among American men and women. Rates of PTSD are much higher in post-conflict settings such as Algeria (37%), Cambodia (28%), Ethiopia (16%) and Gaza (18%).(2)
In a nutshell, Post-Traumatic Stress Disorder (PTSD) is:
• A debilitating anxiety disorder that occurs after experiencing or witnessing a traumatic event that involves either a real or perceived threat of injury or death. This can include a natural disaster, combat, an assault, physical or sexual abuse, or other trauma.
• PTSD sufferers have a heightened sense of danger and impending doom. Their natural “fight or flight response” is damaged, causing them to feel stressed or fearful even in safe situations.
• Once called “shell shock” or “battle fatigue,” PTSD has recently received more public attention because of the high number of war veterans who have the disorder. However, PTSD can happen to anyone at any age. PTSD occurs as a response to chemical changes in the brain and is not the result of a character flaw or weakness.(3)
Symptoms of PTSD
The most common symptoms of PTSD as described by people with its diagnosis are:
- Re-experiencing the trauma through flashbacks; nightmares; obsessive thoughts (they can see, hear, smell, taste things that seem real)
- Insomnia; nightmares
- Intrusive thoughts – thoughts that are unwanted, feel uncontrollable, and often pertain to disturbing or distressing themes
- Concentration problems
- Numbness; depression
- Feelings of estrangement from others; feeling or wanting to be alone
- Hypervigilance – always being on alert; always ready to fight or do battle
- Sudden startling
- Irritability; anger; panic
- Shame; guilt (survivors’ guilt)
- Avoidance of situations, people/objects that remind them of event
- Increased anxiety in general
One of the main reasons that people do not report these symptoms is that these can be easily mistaken for symptoms of mental illness. People often fear that diagnosis, its stigma and all its consequences. Perhaps this is why less than 50% of veterans seek help.
Causes of PTSD
It is important to remember that not everyone who experiences a traumatic event gets PTSD. Many factors come into play. Some of the many causes or risk factors for PTSD are:
- Serious accident, injury; mutilation
- Rape
- Physical, emotional or sexual abuse
- Betrayal by a loved one
- Wars/Attacks/Bombings
- Community violence (shootings/bullying)
- Loss of family members, friends, community, property, possessions, home
- Loss of job
- Natural disasters – tornadoes, hurricanes, earthquakes, fires, flood
Additional risk factors for the development of PTSD include:
- How intense the trauma was or how long it lasted
- If you were injured or lost someone important to you
- How close you were to the event
- How strong your reaction was
- How much you felt in control of events
- How much help and support you got after the event (4)
Many people who go through a trauma have some symptoms at the beginning. Only some will develop PTSD over time. Being exposed to violence as a child as well as a family history of mental illness, depression, mood disorders or anxiety may increase the risk of developing PTSD after a traumatic event. A recent study suggested that the roots of PTSD may not be the battlefield, but in childhood where emotional problems and traumatic events were experienced. The level of violence in a person’ life prior to military experience seemed to be more of a causative factor in the development of PTSD than exposure to combat or other war atrocities.(5)
Vicarious trauma
People with PTSD are not the only ones who are affected by trauma. Those in the helping professions such as medical personnel, doctors, nurses, first responders, emergency workers, fire fighters, police, therapists, social workers, reporters and even energy workers can experience the effects of trauma vicariously because of an empathic connection with the person. Being committed and/or responsible for helping others, seeing suffering every day, being repeatedly exposed to horrific trauma or inhumane acts committed on another human being can eat at the soul or spirit of those trying to help. Hope can be lost and “compassion fatigue” can set in, oftentimes leading to burnout. The person who was dedicated to helping others loses hope and can also become depressed him or herself. Even Reiki practitioners, because of their compassion and energetic connection, can develop compassion fatigue from listening to and working with those experiencing trauma over a long period of time.
Fight or Flight Response
Our bodies are designed for survival and have three responses to stress: Fight, Flight or Freeze. When we perceive a threat, stress hormones are released to activate the body’s protective mechanisms. Often this is referred to as an adrenalin rush. Blood flow to the muscles increases, blood pressure and pulse rates increase, and breathing becomes faster—all to enable the person to respond to the perceived danger. Any function that is not needed for immediate survival either slows down or shuts down. Digestion slows down, the immune response is suppressed, hunger diminishes, etc. Repeated exposure to stress or a stress response sustained over a long period of time can have a damaging impact on one’s health. It can also lead to negative coping mechanisms such as excessive smoking, eating or drinking, numbing through drugs or other maladaptive behaviors. For the person with PTSD, the perception of danger is a constant, and they are always “on.” The body is thus constantly stressed and health problems can develop as a result.
War: A rite of passage
In the past, going to war to protect the tribe, the family or the nation was often seen as a rite of passage. Many cultures had physical, mental and spiritual rituals to prepare their young boys for war. The rite of passage from young boyhood into manhood by going into battle was viewed as an integral part of life. Boys were taught to surrender their ego for the greater good.
When the battle was over, they were welcomed back as men. There were many rituals of return: purification, cleansing and celebration. The “men” were encouraged to tell their story as a way to clear, heal, grow and move on.
War today is much more destructive on many levels and has lingering effects physically and emotionally. Chemical warfare, bombings and other forms of attack can affect soldiers while in battle as well as after they return home. The concept of battle as a rite of passage may exist to a degree, but the return is much different. Soldiers often come back to a culture of denial (remember the Vietnam War). Rituals for healing may be non-existent and vets are often isolated with no sense of community. They don’t get to tell their story as a form of healing. Denial is the name of the game. Perhaps this contributes to the development of PTSD?
Injury to the soul
PTSD can develop after an injury to the soul. The primal urge to survive dominates the human experience. In times of crisis or trauma, a person may often do anything to survive. A person being robbed or raped, assaulted or beaten, may surrender or give in just to stay alive. In times of war or battle, innocent people may be killed, horrific things may be done to another human being or a soldier can survive an attack when others in his or her command didn’t.
The soul knows the difference between good and bad, right and wrong. The above are examples of good people being caught in impossible dilemmas. The things they do to survive may be at odds with their core ethical and moral beliefs. A person may have to go against his or her conscience and find it challenging to believe in his or her own worth and goodness afterwards. Shame and guilt may follow, contributing to the development of PTSD as well.
The energetic dynamics of trauma
Looking at the energetic chakra system, you can see that trauma can affect a person at any level. Using Byosen scanning or a pendulum to detect the area most out of balance or in need at that moment is perhaps the best way to begin. Any trauma to that part of the body or what it represents can affect the person physically, emotionally, mentally or spiritually. Here are some examples:
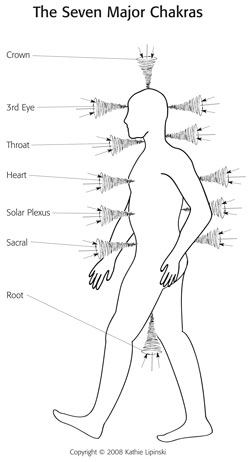 The First Chakra/ Root Chakra has to do with safety and survival, one’s family of origin or “roots.” Any threat to one’s survival be it a natural disaster, attack, loss of job, home, family dysfunction or act of violence
The First Chakra/ Root Chakra has to do with safety and survival, one’s family of origin or “roots.” Any threat to one’s survival be it a natural disaster, attack, loss of job, home, family dysfunction or act of violence
The Second Chakra/ Creative or Sacral Chakra has to do with creativity, sexuality or intimacy. Some say it is also represents where we store our emotions. Any threat to or attack of a sexual nature, any loss of physical function, or betrayals of intimacy
The Third Chakra/ Solar Plexus or Power Center Chakra represents our personal power and its expression. Any attack that attempts to take away one’s power or make one submissive.
The Fourth Chakra/ or Heart Chakra has to do with love: love of self, love of others. Loss of love, loss of a loved one, betrayal, hurtful words or actions
The Fifth Chakra/ or Throat Chakra has to do with communication. Do you speak up for yourself; are your words suppressed; are you allowed to speak or often silenced?
The Sixth Chakra/ or Third Eye Chakra has to do with intuition or knowing. Do you trust what you sense or know? Do others negate or ridicule your “knowing”? Has life led you to distrust your intuition? Has something bad happened because you didn’t listen to your inner voice?
The Seventh Chakra/ or Crown Chakra relates to spirituality and feeling connected to a higher power; Source. Have you lost faith or trust in life? With your fellow human being? Do you feel alone in the world? Not connected?
How Reiki can help when working with PTSD
Reiki, simply stated, calms and stills the spirit of the person. It can promote relaxation from the outside in and remind the body how it feels to be calm again. The act of sharing Reiki can also remind the body that physical touch can be nurturing and therapeutic. Reiki promotes inner peace and calm. When the spirit self has been calmed and quieted, the physical healings of the body can begin.
During the fight or flight response, emotions are often buried in an attempt to assist the person through the traumatic experience. Oftentimes, emotions can get trapped and stored in the body as cellular memory. Through deep relaxation and calming of the spirit, those trapped or buried emotions and trauma can be gently released.
It is important to remember that Reiki heals at the soul or spirit level, thus we can never predict the person’s experience or outcome. Trusting and following the energy will always take us where we need to go and address what the person needs most in that moment.
Reiki and PTSD
Reiki students and practitioners often ask me “what is the protocol for” or “how should I work with a person with …”? My answer is always that you follow the energy. When a person comes to you, no matter what the diagnosis or condition is, you treat them as a human being first. People are not their diagnosis or their condition. Understanding the condition or having guidelines can help (see working with PTSD Guidelines), but the most important thing to know when giving Reiki is that it acts on priority. This means that it gives the person what they most need at that moment in time….not what we think they need. The person may need physical relaxation, emotional calming, mind clearing, etc. They may need to release old traumas. We don’t know and should not assume we know what they need. Let the person and his energy guide you and show you what he needs.
Reiki at the VA: The Innovations in Care Grant
This past year I was privileged to be part of the Innovations in Care Grant at the Northport VA Medical Center on Long Island. The grant was part of a national movement toward wellness, health coaching and self-care for veterans. Richelle Rappaport, RN, MSN, AHN-BC, PMHCNS-BC, was responsible for writing the grant. The focus of the program was to train VA Clinical staff in various holistic modalities including Reiki, meditation, guided imagery, Tai Chi and reflexology. (Her description of the grant and its stages is featured in the current issue of Beginnings: Journal for the American Holistic Nurses. The issue was dedicated to holistic nurses joining forces to care for veterans(6). I began teaching Reiki I and II to the VA staff in October 2011 and completed the training in June 2012. Those that attended were mostly nurses, but several social workers, physical therapists, psychiatrists, one medical doctor, pharmacists, occupational therapists and several nursing assistants also attended. Classes were held at the VA and more than 60 personnel completed Reiki I and II. Those that had already had Reiki II were advanced to Advanced Reiki Training and the Master Teacher level. They were so willing and excited to learn Reiki and marveled at this simple yet powerful technique. It was such a gift to bring this wonderful healing energy to the staff so that they could take care of themselves as well as their patients. Since completing the training, many are using it in their personal lives to take care of themselves and their loved ones. Some are blending it in with their patient care on their perspective units and sharing it among themselves.
Reiki for vets
Since the Innovations grant began, nurses and other health care professionals who have provided Reiki have shared some of the comments from vets after their sessions. Here is what the vets said:
“The Reiki helps me sleep through the night.”
“I can focus better and I am looking at life more positively.”
“I have not had a panic attack in four weeks and have not awoken with a nightmare.”
“The Reiki helps me to be more open with my wife. I am talking more.”
“I can relax now and I am sleeping better.”
“I had two to three panic attacks a week when we began. I have not had any in weeks.”
“The Reiki helps my headaches. I am decreasing my pain meds with my doctors’ direction.”
“I have never showed any emotion related to my survivor guilt. The Reiki helped me to let the emotions out.” (Vietnam vet)
“I can’t believe my pain is decreased. The narcotics can’t do that.”
“I have not been able to relax since Iraq. The Reiki allows me to relax for the first time.”
“I have started to do things I always wanted to do. I am no longer doing things I should not do. I am letting things go and not getting angry about everything. I am becoming who I really am.” I am like a caterpillar changing into a butterfly.”
“Reiki helps me go to a place of peace inside.”
A patient, who could not sit still, sat quietly for 30 minutes and reported that his back pain went from a 10 down to a 6. A woman who had PTSD after 9/11, reported that she felt “more trusting” after her Reiki sessions. Her Reiki session was like a “safe haven” for her.
Guidelines for Reiki practitioners working with clients with PTSD
Based on our experiences working with the vets at the VA (but relevant for consideration for anyone with PTSD), here are some suggestions to keep in mind:
- Reiki is about relaxation and balancing energy
- It is not our job to fix them; we hold the space for healing
- Do not diagnose
- Follow the energy and allow yourself to be guided
- Don’t practice beyond your training
- Create a sense of safety and trust (very important)
- Be honest
- Educate yourself about PTSD
- PTSD needs a holistic approach (combination of Reiki, medications and talk therapy)
- Have a therapist you can refer clients to. Have one that you can confer with if you have questions
- Start slowly; work on establishing trust and safety
- It’s important for them to feel in control
- Ask for permission to touch.
- May begin with hands 1–2 inches off the body until person feels comfortable with touch
- Ask “What would make you more comfortable?”
- Leave door open; let client face the door; may not like others watching
- Be mindful of music – eg. some Vietnam vets don’t like Asian music
- No woo woo stuff. Vets are most often very down-to-earth people.
- Don’t press them to tell their story—this can re-traumatize them
- Look them in the eyes; call them by their name. Respect is important to them
- Offer your full presence; focus on the moment
- Let them know it is okay if they want to keep their eyes open during a session
- Don’t stand behind them without telling them—NO SURPRISES!!
- Check in with them often during session
- Let them set the pace
Most important: JUST DO REIKI!
How to handle a flashback
When working with someone who has PTSD or has undergone a serious trauma, flashbacks— or the reliving of an intense experience—may happen. These flashbacks can be happy or sad, exciting or any other emotion. The problem is that the person may not be able to recognize it as a memory and believe that it is happening now. Here are some guidelines on what to do if a person has a flashback.
- Break contact and take your hands off the person immediately
- State the person’s name; orient him or her as to place and time (“Joe, this is …and you are in my office for a Reiki session”)
- Make eye contact; have the person look at you or something in your office
- Ask him or her to sit up
- Don’t assist or touch without permission
- Move to the side and do not sit or stand above him or her
- Have the person count out loud
- Give the person space and time to come back
Summary
After my presentation at the Retreat, participants were interested in how they could gain access to the VA system to help get Reiki to the vets. I explained that not all vets want to access the VA system to get help. Some want nothing more to do with the military once their tour is done. Others don’t want to be labeled as PTSD as it can affect their work record. There are many vets in the community not utilizing VA services. I have provided a list of resources (See Resources) such as Honor A Veteran to help veterans in your area. People with PTSD can be found in various support groups like 12 Step programs, TBI groups (Traumatic Brain Injury), mental health facilities and local veterans associations.
PTSD is a complex condition and many people will have to deal with it sometime in their life or the life of a loved one. The more we know about it, the more we can understand and help. Public awareness of PTSD is on the rise and there is so much information and so many resources now available. Reiki is a great way to calm and nurture the spirit of someone experiencing PTSD.
Reiki and PTSD Resources List
Books
Curtin, Richard. 2012. Psychotherapeutic Reiki, A Holistic Mind Body Approach To Psychotherapy – A Training Manual. Lulu.com.
Hart II, Ashley B. 2000. An Operators Manual for Combat PTSD: Essays for Coping. Iuniverse.
Levine, Peter. 1997. Waking the Tiger: Healing Trauma: The Innate Capacity to Transform Overwhelming Experiences. Berkeley, CA: North Atlantic Books.
Levine, Peter. 2010. In an Unspoken Voice: How the Body Releases Trauma and Restores Goodness. Berkeley, CA: North Atlantic Books.
Naparstak, Belleruth. 2005. Invisible Heroes: Survivors of Trauma and How They Heal. New York, NY: Bantam. www.HealthJourneys.com.
Tick, Edward. 2005. War and the Soul: Healing Our Nation’s Veterans from Post-Traumatic Stress Disorder. Wheaton, IL: Quest Books.
Articles
Fehrs, Linda. "Reiki and psychological trauma." Institute for Integrative Healthcare Studies. www.integrative-healthcare.org.
Dey, Eileen, and Michael Emanuel. :Reiki for veterans." Reiki News Magazine Winter2008: 41—43.
"Holistic nurses joining forces to care for veterans." Beginnings: Journal of the American Holistic Nurses 32 no. 5. (October 2012): 14—16. www.ahna.org.
Websites
http://www.nimh.nih.gov/health/publications/post-traumatic-stress-disorder-ptsd.
The National Institute for the Clinical Application of Behavioral Medicine. www.nicabm.com.
www.vetcenter.va.gov. 300 centers in United States. 877-WAR-VETS (927-8387).
Honor a Veteran. Holistic services free or at discount rate for vets and families. http://honor-a-veteran.org.
Warrior Transition Unit. www.crdamc.amedd.army.mil/newSite/behav-health/rr-ctr.aspx.
Endnotes
2 http://www.ptsd.va.gov/professional/pages/ptsd-overview.asp.
3 http://www.healthline.com/health/post-traumatic-stress-disorder.
4 http://www.ptsd.va.gov/public/.
5 Wray, Herbert, “Embattled Childhood: The Real Trauma in PTSD,” Scientific American Mind (Nov/Dec 2012): 74.
6 “Holistic Nurses Joining Forces to Care for Veterans,” Beginnings: Journal of the American Holistic Nurses 32, no. 5 (October 2012): 14 – 16, www.ahna.org.







